On September 7, 2016, the Food and Drug Administration (FDA) warned women and their doctors that current tests being marketed as ovarian cancer screening tests are unreliable and could lead to false diagnoses.
Summary of the Problem:
The FDA described the problem in their recent safety communication as follows:
Despite extensive research and published studies, there are currently no screening tests for ovarian cancer that are sensitive enough to reliably screen for ovarian cancer without a high number of inaccurate results. However, over the years, numerous companies have marketed tests that claim to screen for and detect ovarian cancer.
For example, recently, Abcodia Incorporated began marketing the Risk of Ovarian Cancer Algorithm (ROCA) test in the United States, with claims that the ROCA test can screen for and detect ovarian cancer before symptoms appear and increase the chance for survival. Yet, available data do not support its claims.
FDA is concerned that women and their physicians may be misled by such claims and rely on inaccurate results to make treatment decisions. Based on the FDA’s review of available clinical data from ovarian cancer screening trials and recommendations from healthcare professional societies and the U.S. Preventive Services Task Force, available data do not demonstrate that currently available ovarian cancer screening tests are accurate and reliable in screening asymptomatic women for early ovarian cancer. For example, some women may receive test results that suggest ovarian cancer even though no cancer is present (a false-positive). These women may undergo additional medical tests and/or unnecessary surgery, and may experience complications related to both. Or, test results may not show ovarian cancer even though cancer is present (a false-negative), which may lead women to delay or not seek surgery or other treatments for ovarian cancer.
Using unproven ovarian cancer screening tests also may be harmful for women with increased risk for developing ovarian cancer. For instance, these women and their doctors may not take appropriate actions to reduce their future risk if they rely on a result that shows no cancer currently present. Yet, this group of women is still at high risk of developing ovarian cancer later based on their gene mutation and/or family history. The FDA believes that women at high risk for developing ovarian cancer should not use any currently offered test that claims to screen for ovarian cancer.
Screenings for breast, colon and cervical cancers are successfully used for early detection and prevention of cancer-related deaths. At this time, the FDA is not aware of any valid scientific data to support the use of any test, including using a test cleared or approved by FDA for other uses, as a screening tool for ovarian cancer. Any safe and effective ovarian cancer screening test would have to take into consideration the particular way in which this cancer progresses. Unlike other cancers, this type of tumor has no pre-cancer that is currently detectable without invasive surgery, and it usually spreads to other parts of the abdominal cavity before it is discovered.
5th Leading Cause of Cancer-Related Deaths in Women:
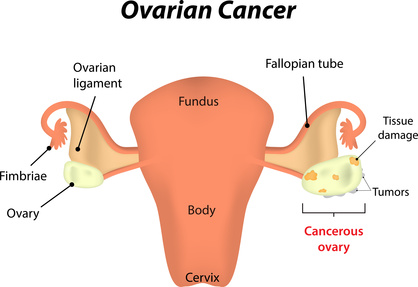
Ovarian cancer occurs when abnormal cells in or near the ovaries grow and form a malignant (cancerous) tumor. As described in the FDA’s safety communication, in the United States, ovarian cancer is the fifth leading cause of cancer-related death among women. The National Cancer Institute estimates that in 2016, more than 22,000 women will be diagnosed with ovarian cancer. Women who have reached menopause, women who have a family history of ovarian cancer, and women with the BRCA1 or BRCA2 genetic mutations have the highest risk for developing ovarian cancer.
The FDA’s Recommendations:
The FDA makes the following recommendations for women and their physicians:
For women, including those at increased risk of developing ovarian cancer:
- Be aware that there is currently no safe and effective ovarian cancer screening test.
- Do not rely on ovarian cancer screening test results to make health or treatment decisions.
- Talk to your doctor about ways to reduce your risk of developing ovarian cancer, especially if you have a family history of ovarian cancer, or have the BRCA1 or BRCA2 genetic mutations.
For physicians:
- Do not recommend or use tests that claim to screen for ovarian cancer in the general population of women. Be aware that testing higher risk asymptomatic patients for ovarian cancer has no proven benefit and is not a substitute for preventive actions that may reduce their risk.
- Consider referring women at high risk of developing ovarian cancer, including those with BRCA mutations, to a genetic counselor or gynecologic oncologist, or other appropriate health care provider for more specialized care.
Attorney Pamela A. Borgess, the founder of Borgess Law, LLC, is an experienced trial attorney who focuses on civil litigation, including mass torts/class actions, defective medical drugs/devices, defective consumer products, business/contract disputes, wrongful death and injury, car and truck accidents, and nursing home abuse cases. To speak with Attorney Borgess, call Borgess Law, LLC at (567) 455-5955 or toll-free at (844) LAW-9144. You can also contact Borgess Law, LLC by submitting an online inquiry. Borgess Law never charges for initial consultations.